Even if you have normal blood sugar, chronically high insulin could be the culprit behind some of the health issues you may be dealing with—like migraines, hypertension, cardiovascular disease, and so many more.
In the keto community, we put a lot of emphasis on maintaining healthy blood sugar levels, and rightly so. After all, more than 38 million people in the US have diabetes (95% of which is type 2), and this condition is a leading cause of blindness, kidney failure, cardiovascular disease, and amputations.
But does normal blood sugar guarantee good metabolic health? What if you’re living with unexplained health problems despite normal blood sugar? Could something be causing poor cardiometabolic health even if you don’t have diabetes or prediabetes? Yes. It’s time to shift the focus to insulin. Specifically, to hyperinsulinemia – chronically elevated insulin.
- What is chronic hyperinsulinemia?
- Is hyperinsulinemia the same as high blood sugar?
- Why is hyperinsulinemia a problem?
- Is hyperinsulinemia the same as insulin resistance?
- How do you test for hyperinsulinemia? What is a normal insulin level?
- Hyperinsulinemia and metabolic syndrome
- Is keto good for hyperinsulinemia?
- Bottom line
- Looking for a low-carb meal?
What is chronic hyperinsulinemia?

The meaning of the phrase chronic hyperinsulinemia is built right into it:
Chronic: constant, habitual
Hyper: high, over, or elevated
Insulin: the hormone insulin
-Emia: in the blood
So, chronic hyperinsulinemia means that the level of insulin in your blood is too high, too often.
Is hyperinsulinemia the same as high blood sugar?

A blood glucose (a.k.a. blood sugar) measurement tells you the concentration of the simple sugar glucose in your blood. Insulin is a hormone that plays a role in regulating blood sugar, but it is entirely different from glucose. So, high insulin is not the same thing as high glucose.
Glucose and insulin levels don’t always track together. If you have normal or low blood sugar, you can’t automatically assume that your insulin level is also normal or low. It’s possible to have little to no insulin with very high blood sugars (as in type 1 diabetes), and very high insulin with completely normal blood sugar.
Why is hyperinsulinemia a problem?
Insulin is commonly thought of as a “blood sugar hormone,” and it’s true that insulin helps to lower blood sugar. But insulin has many other roles unrelated to blood sugar. In fact, one of insulin’s most powerful effects is that it inhibits lipolysis. That’s the technical term for saying it gets in the way of breaking down fat.
(In our book End Your Carb Confusion, keto authority Dr. Eric Westman and I explained that insulin is like a security guard that stands outside your fat cells and makes sure the stored fat doesn’t escape.)
Insulin also promotes fat storage, so it’s a double whammy: insulin stimulates your body to store fat and then keeps it sequestered away. This is partly why chronically high insulin can make it difficult to lose weight, and why dietary approaches that help to lower insulin – like a keto diet – facilitate weight loss.
Insulin is also considered to be an anabolic hormone, meaning that it helps things grow and get larger. Because of this growth-promoting effect, hyperinsulinemia is associated with obesity, enlarged prostate (BHP, a.k.a. benign prostate hyperplasia), skin tags (excess skin growth), and certain types of cancer (unchecked cell growth).
Beyond those, owing to other signaling effects of insulin separate from its effect on blood sugar, chronic hyperinsulinemia is believed to be a major cause or exacerbating factor in:
- Cardiovascular disease
- Dyslipidemia (low HDL-cholesterol & high triglycerides)
- Polycystic ovarian syndrome (PCOS)
- Non-alcoholic fatty liver disease
- Hypertension
- Alzheimer’s disease
- Skin problems
- Migraine
- Erectile dysfunction
- Inner-ear & balance disorders (e.g., vertigo, tinnitus, Ménière’s disease)
Note that except for type 2 diabetes, none of the conditions caused or made worse by hyperinsulinemia are characterized by high blood sugar. So, even if you have normal blood sugar, chronically high insulin could be the culprit behind some of the health issues you may be dealing with.
Is hyperinsulinemia the same as insulin resistance?

This is a hotly debated question! Some experts say that insulin resistance comes first. That is, if your cells are resistant to the actions of insulin, then your pancreas has to secrete more insulin in order to make the signal stronger, which would mean that insulin resistance causes hyperinsulinemia.
Others argue that insulin resistance is the result of hyperinsulinemia: a chronically high insulin level causes the body to become resistant to the hormone – to stop listening to it.
Researchers and academics might define hyperinsulinemia and insulin resistance differently, but if your main interest is maintaining good health or reversing any cardiometabolic problems you’re currently living with, then it’s largely a semantic difference and you can consider them to be the same.
How do you test for hyperinsulinemia? What is a normal insulin level?
There’s no official test for chronic hyperinsulinemia, but you can measure your fasting insulin level with a simple blood test. The chemical assay used to measure insulin in the blood is more complicated than the one for measuring glucose, so at this time there are no monitors for measuring insulin at home, but researchers are working on this.
What is a normal fasting insulin level? Different labs use different ranges, but they’re typically in the ballpark of 2.6-24.9 µIU/mL. Most keto-oriented medical and nutrition professionals agree that conventional reference ranges for fasting insulin are too generous.
Most prefer fasting insulin to be below 10 µIU/mL, and some would say that under 5 µIU/mL is ideal. It’s difficult to pinpoint what’s optimal for any one individual, but most keto professionals would agree that if your fasting insulin is in the double digits, it’s too high.
If your fasting insulin level is significantly elevated, that’s a sign that you might have chronically high insulin, but fasting insulin is a bit volatile: one elevated measurement doesn’t automatically indicate a problem, just as one elevated glucose reading isn’t automatically cause for concern.
(And like fasting glucose, it’s not uncommon to have a normal fasting insulin level, but insulin might rise abnormally high after a meal – especially a high-carb meal – and stay elevated for a longer time than normal. Under this circumstance, you would experience the adverse effects of elevated insulin but the problem wouldn’t be revealed by measuring your insulin level in a fasted state.)
One way to know what’s happening to your insulin level after a meal is to do an oral glucose tolerance test (OGTT) that includes measurements of insulin. The standard OGTT lasts for just two hours and measures only glucose, but there’s a more advanced test that extends to five hours and measures both glucose and insulin. This is called the Kraft test, and it was pioneered by Joseph Kraft, MD.
After seeing thousands of OGTTs that included insulin measurements, Kraft became one of the first people to identify the hidden problem of high insulin in people with normal glucose, and to make the connections between hyperinsulinemia and type 2 diabetes, cardiovascular disease, and other health problems. (If you’d like to learn more, I recommend Dr. Kraft’s book, Diabetes Epidemic & You.)
Should you drink pure liquid glucose?

As a keto nutritionist, I don’t recommend that anyone drink pure liquid glucose for the sake of measuring insulin unless this is deemed medically necessary.
(Plus, if you’re already following a keto diet, it’s recommended that you “carb up” by eating at least 100 grams of carbs a day for a week before taking an OGTT so that you don’t have a false result. And if you’ve been getting great results from keto, why would you want to do that? Moreover, if you do have chronic hyperinsulinemia, keto is one of the most effective ways to correct it, so you’re already taking action to improve things.)
So, if your fasting insulin level is normal, how can you tell if you have hyperinsulinemia?
You can infer that you have chronic hyperinsulinemia based on indirect clues, like some of the conditions mentioned earlier, or if your doctor has told you that you have metabolic syndrome.
If your fasting insulin is high and you also have signs of metabolic syndrome or you’re living with one or more of the conditions mentioned earlier, then you’d be right to suspect that hyperinsulinemia might be the underlying factor.
Hyperinsulinemia and metabolic syndrome

There may be shades of gray between hyperinsulinemia and insulin resistance, but whatever you call it, chronically elevated insulin is the driving force behind metabolic syndrome.
Metabolic syndrome is diagnosed if you have three or more of these five criteria:
- Large waist circumference: > 35 inches (89 cm) for women; > 40 inches (102 cm) for men
- High triglycerides: > 150 mg/dL (1.7 mmol/L)
- Low HDL: < 50 mg/dL (1.3 mmol/L) for women; < 40 mg/dL (1.04 mmol/L) for men
- Hypertension: ≥ 130/85 mmHg
- Elevated fasting glucose: ≥ 100 mg/dL (5.6 mmol/L)
(Some researchers have suggested that elevated uric acid should be added to the metabolic syndrome diagnostic criteria, as I mentioned in a past article.)
So you can see that even if your fasting blood sugar is normal, if you have three of the other criteria, you would be classified as having metabolic syndrome. You might also notice that fasting insulin isn’t included in the diagnosis.
This might be a reflection of how volatile fasting insulin can be (it’s not worth including if it’s so unreliable), but considering that fasting glucose is included (which is equally volatile), it’s more likely indicative that conventional medicine has a ways to go in acknowledging the influence of hyperinsulinemia or insulin resistance in so many of the chronic, non-communicable diseases that affect millions of people.
It’s also worth noting that while waist circumference is included in diagnosing metabolic syndrome, body weight is not. This means you can have metabolic syndrome or hyperinsulinemia even you’re not overweight or obese. Being at a “normal” body weight means nothing when it comes to metabolic health.
Millions of people with type 2 diabetes or prediabetes, PCOS, BPH, erectile dysfunction, hypertension, and other manifestations of insulin resistance, fall all along the spectrum of body weights and sizes. Not all are overweight or obese.
Is keto good for hyperinsulinemia?

The main thing that leads to elevated insulin is elevated blood sugar. So, an effective way to prevent very large rises in insulin is to prevent large rises in blood sugar. (Protein has a small effect on insulin, too, but it’s minor compared to the effect of refined carbs.) And since keto diets eliminate the foods that tend to raise blood sugar the most, keto is powerful for maintaining lower insulin levels.
Type 2 diabetes is the end stage of insulin resistance – when the pancreas is still secreting large amounts of insulin but the cells are so resistant to it that they are no longer able to accept additional glucose from the bloodstream. And we know that keto is a slam-dunk for reversing type 2 diabetes, so it stands to reason that keto is good for improving the underlying insulin resistance.
And while many medical professionals think weight loss is required in order to improve insulin sensitivity or reverse metabolic syndrome and type 2 diabetes, research shows that keto diets can reverse metabolic syndrome and improve type 2 diabetes and insulin sensitivity even without clinically significant weight loss.
Many thousands of people who follow keto diets can attest that their fasting insulin level decreased substantially after they cut the carbs. For some people it happens very quickly but for others it can take a bit longer. If you’re following a keto diet but your fasting insulin is still elevated, be patient. You might be one of the people for whom it just takes a little more time.
Plus, since fasting insulin isn’t a standard test, then after you started keto might be the first time you’ve ever had it measured, so you have no prior data to compare to. It’s possible that the still-elevated level is actually a big improvement over where it was before you started keto, and it will continue to get better over time.
(As mentioned earlier, fasting insulin isn’t an ironclad measurement, but I think it’s worth including in your routine blood work on a keto diet.)
Bottom line

Chronically elevated insulin is the main driver of numerous health issues even when your blood sugar is normal. There are ways to measure your insulin, both fasted and after a bolus of carbohydrate, but you can use indirect clues as evidence that you likely have hyperinsulinemia.
Some of these include being diagnosed with metabolic syndrome or insulin resistance, PCOS, gout, non-alcoholic fatty liver disease, or BPH. If you have hyperinsulinemia or insulin resistance, a keto diet can help to correct the underlying metabolic dysfunction and restore normal insulin levels.
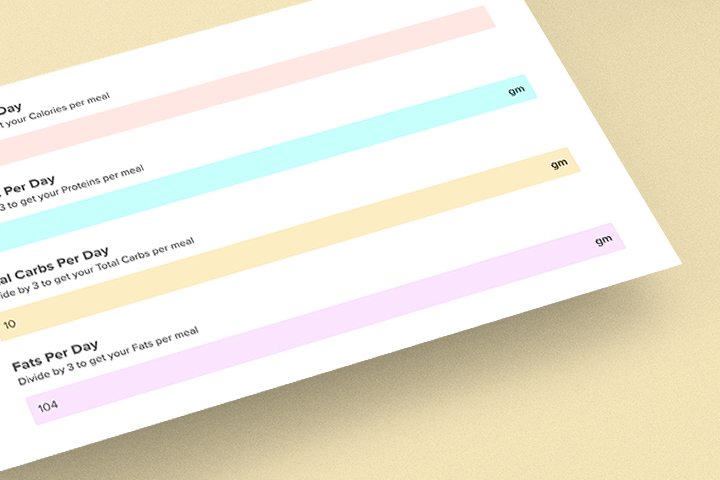
Looking for a low-carb meal?
Then check out Keto Chow! Keto Chow is a keto-friendly meal with 1/3 of your daily recommended nutrients. It can be made in seconds, and you can choose from over 25 delicious flavors!