Let me say this in plain English: cutting carbs and increasing fat is a simple and safe treatment for PCOS.
Do you have PCOS or know a woman who does? Chances are you do, because PCOS is the most common endocrine problem among women of reproductive age, affecting approximately one in ten women or at least ten million women worldwide.
Despite the name – polycystic ovarian syndrome – many women with the condition don’t actually have cysts in their ovaries, so let’s take a closer look at what PCOS really is and how a keto diet can help.
PCOS Basics

PCOS is a major cause of infertility, menstrual irregularity, and reduced quality of life in reproductive aged women, and many of the women living with it might not even know they have it.
The condition results from a cluster of hormonal abnormalities, namely, elevated insulin, elevated androgens (male characteristic sex hormones), and often, reduced progesterone. These hormonal irregularities are responsible for the signs and symptoms of PCOS.
The most common signs and symptoms of PCOS are:
- Weight gain; obesity
- Acne; oily skin
- Irregular or absent periods
- Infertility or difficulty getting pregnant
- Mood swings
- Pelvic pain
- Excess androgens (especially testosterone)
- Anovulatory menstrual periods (bleeding without ovulation)
- Hair loss on the head or thinning of hair on the head
- Hirsutism (excess body hair) – particularly facial hair, but may also include hair on the chest, back, abdomen, and arms
The reason PCOS is classified as a “syndrome” is that there’s no single definitive diagnostic test like there is for certain bacterial and viral infections. PCOS is diagnosed based on a constellation of signs and symptoms, usually corroborated by blood tests to detect the hormonal imbalances mentioned above.
Insulin and PCOS

The primary cause of PCOS is chronically elevated insulin (hyperinsulinemia). Researchers are cautious in how they state things in their publications. They rarely state definitively that something is the cause of something else.
They prefer to use phrases like “associated with” or “linked to.” In the case of hyperinsulinemia and PCOS, though, at least one group of authors was more forthright and said, “Hyperinsulinemia associated with insulin resistance has been causally linked to all features of the syndrome, such as hyperandrogenism, reproductive disorders, acne, hirsutism and metabolic disturbances.” (Emphasis added.)
Women with PCOS may be told that because they have PCOS, they’re at increased risk for type 2 diabetes, metabolic syndrome, cardiovascular disease, hypertension and other issues. But it’s actually the other way around: women with PCOS already have insulin resistance. Insulin resistance led to the PCOS, and insulin resistance also increases risk for type 2 diabetes, cardiovascular disease, and high blood pressure.
PCOS doesn’t cause those other conditions to develop; PCOS is simply a manifestation of insulin resistance, just as all those other conditions are.
This is key information to have, because if you know the root cause, then it’s easier to find the most effective treatment.
(This image is a nice summary of how hyperinsulinemia affects the ovaries, adrenal glands, liver, brain, leading to the hormonal imbalances that characterize PCOS.)
PCOS and Body Weight

PCOS often comes along with being overweight or obese, but not always. Only about half the women with PCOS are overweight, so if a slimmer woman is living with key indicators of this condition, the possibility that she has it shouldn’t be dismissed just because she isn’t carrying extra weight.
Researchers have identified “profound insulin resistance” in PCOS patients who are obese as well as those who are lean. Women with PCOS have been found to “have significant insulin resistance” independent of their weight.
To the extent that chronic hyperinsulinemia causes PCOS, let’s remember that body weight is not included in the diagnostic criteria for metabolic syndrome (a.k.a. insulin resistance). The signs and symptoms of metabolic syndrome – and PCOS – can occur in people all across the weight spectrum.
Researchers note “that both obese and lean women with PCOS have some degree of insulin resistance. Insulin resistance is implicated in the ovulatory dysfunction of PCOS by disrupting the hypothalamic-pituitary-ovarian axis.”
Here again researchers came right out and said that insulin resistance is implicated in the irregularities in the menstrual cycle by adversely affecting other hormones. So it stands to reason that correcting the underlying hyperinsulinemia could have a beneficial impact on PCOS. And that’s exactly what the research shows.
Keto Diets and PCOS

The first study on a ketogenic diet in women with PCOS was done by well-known keto authority Dr. Eric Westman and colleagues. It was a small pilot study – just five subjects – but the results were so impressive that it’s worth looking at. Subjects were overweight or obese women with PCOS who were instructed to follow a strict keto diet – no more than 20 total grams of carbohydrate per day for six months.
(They were given the food list Dr. Westman uses in his clinic at Duke University – it’s the same as the Phase 1 food list in the book we co-authored, End Your Carb Confusion.)
Here’s what happened to the women after following the keto diet:
- Body weight: -12%
- Percent free testosterone: -22%
- LH/FHS ratio: -36%
- Fasting insulin: -54%
Their fasting insulin dropped by more than fifty percent, along with substantial decreases in other hormones or imbalances that contribute to the signs of PCOS. Not only that, but two of the subjects got pregnant despite previous struggles with infertility! (As mentioned earlier, PCOS is a major cause of infertility, accounting for as much as 80% of anovulatory infertility cases, and 70 to 80 percent of women with PCOS experience infertility.)
A more recent study looked at outcomes in overweight and obese women with PCOS who followed a low-starch, higher fat diet for 8 weeks. Subjects were told to eat ad libitum (they were not told to restrict calories or even to count carbs), and they were also told not to change their physical activity.
After 8 weeks, the subjects lost weight, lost about 3 inches off their waist circumference, had lower total testosterone, and had significant decreases in fasting and post-meal insulin. This study is encouraging because it shows that impressive results can happen without counting calories or increasing exercise. (So much for “eat less, move more!”)
Some other studies

A recent meta-analysis looking at ten clinical trials including over 400 women with PCOS concluded that ketogenic diets decreased triglycerides, fasting glucose, HOMA-IR (a marker of insulin resistance), total cholesterol and LDL, plus a significant decrease in luteinizing hormone and total testosterone levels, with an increase in follicle-stimulating hormone – all of which indicate improved metabolic health and a trend toward normalizing reproductive hormones.
Turning toward fertility, a study from 2023 offered encouraging evidence that a keto diet can improve the likelihood of a successful pregnancy in women with PCOS undergoing in vitro fertilization (IVF) treatment. All subjects were overweight or obese and had been unsuccessful with at least one previous round of IVF.
The study diet called for a daily carb intake of 50 grams or less, and ketosis was confirmed via urine testing. After 14 weeks, the women had lost weight (an average of 17 pounds), and triglycerides, fasting glucose and insulin, and HOMA-IR all decreased.
The results from this study were even more impressive with regard to successful IVF treatment and full-term pregnancies. Compared to their previous IVF cycle, IVF combined with a ketogenic diet led to substantially improved embryo implantation rate (83% vs. 8% for previous cycle), clinical pregnancy, and live birth rates (66% vs. 0%).
The researchers wrote, “Here, restriction in carbohydrate consumption in PCOS patients induced ketosis, improved key metabolic parameters, and decreased IR. Even though this did not affect oocyte or embryo quality or quantity, the subsequent IVF cycle significantly improved embryo implantation and pregnancy rates.”
Adopting keto for PCOS

For women with PCOS who have been unsuccessful with fertility treatments, adopting a keto diet (with or without additional fertility treatments, under medical guidance) could potentially increase the odds of a successful pregnancy.
For women with PCOS who aren’t ready to go full-on keto, just cutting carbs can be helpful. A study in obese women with PCOS showed that keeping protein constant, going from a diet that was 60% carbs and 25% fat to a diet with 40% carbs and 45% fat led to a 30 percent decrease in daylong insulin levels. The authors wrote:
“Replacement of dietary CHO [carbohydrate] with mono/polyunsaturated fat yields clinically important reductions in daylong insulin concentrations, without adversely affecting lipid profile in obese, insulin-resistant women with PCOS. This simple and safe dietary intervention may constitute an important treatment for PCOS.”
Let me say this in plain English: cutting carbs and increasing fat is a simple and safe treatment for PCOS.
Diabetes, Drugs, and PCOS

Metformin – a diabetes drug – is at the top of the list of medications used for PCOS. This alone should clue us in to the connection between insulin resistance and PCOS. Other diabetes drugs have also been shown to help improve relevant hormone levels and restore fertility or help to improve menstrual regularity.
For women who prefer a more natural approach, supplementing with inositol has been shown to help decrease glucose, insulin, and testosterone, and to facilitate weight loss. Moreover, inositol therapy for PCOS has been shown to be about as effective as metformin, with fewer side-effects. (But metformin and inositol can be used together, and the combination has been shown to be more effective than metformin alone.)
What’s inositol? It was once considered to be a vitamin (vitamin B8) but it is no longer classified as an essential nutrient because the human body typically synthesizes an adequate amount. It’s available in two main supplemental forms: myo-inositol (MI) and D-chiro-inositol (DCI).
Supplementation with one or both has consistently been shown to favorably impact the hormonal imbalances characteristic of PCOS. Combining the two seems to induce a bigger benefit than using either alone.
The preponderance of data suggest that combining insulin-sensitizing drugs and supplements is more effective than using individual medications or supplements on their own. It’s important to note, however, that none of this research was done in women following low-carb or ketogenic diets.
We know that keto diets are effective for improving insulin sensitivity and improving fertility and hormone balance in PCOS – without medications or supplements. We don’t know if women with PCOS following a keto diet would derive any additional benefit with regard to their hormones or fertility from taking diabetes medications or supplements.
Bottom Line

Women with PCOS need to know that their condition is driven by chronically high insulin, and whether or not they’re carrying excess body fat, a low carb or keto diet is a dynamite way to bring down insulin levels.
If you are among the one in ten women living with PCOS, consider adopting a very low-carb or ketogenic diet if you’re not already eating this way (as always, in consultation with your healthcare provider). Keto diets are effective for lowering insulin, and lowering insulin is the cornerstone for helping to normalize the other hormone imbalances and metabolic dysfunction responsible for the signs and symptoms of PCOS.
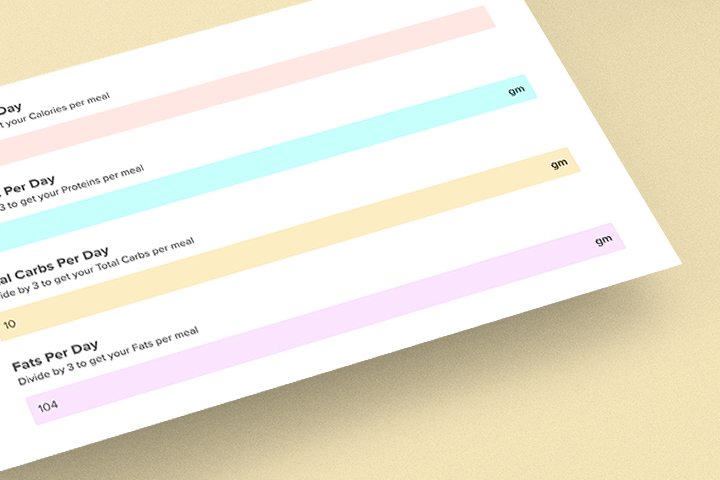
Looking for a keto-friendly meal?
Then check out Keto Chow! Keto Chow is a low-carb shake mix with 1/3 of your daily recommended nutrients, including protein, electrolytes, vitamins, minerals, and more. Choose from over 25 flavors that can be made in seconds.