Anyone interested in optimizing their health can benefit from wearing a CGM. These devices can be a helpful tool to customize your diet because you can clearly see how the foods you choose affect your glucose level.
Continuous glucose monitors (CGMs) can be game-changers for improving your health, but they can be anxiety-inducing if you don’t understand some basics about blood sugar regulation. So let’s take a closer look at CGMs: what are they, who should use them, and what are the finer points you need to be aware of so that you can get helpful information from them without making yourself crazy?
What is a CGM?

CGMs are devices that measure the level of glucose in your interstitial fluid – the non-blood liquid surrounding your cells. This is different from conventional glucometers, which measure the glucose level in capillary blood. So, CGMs detect your glucose level, but it’s not technically your blood glucose level.
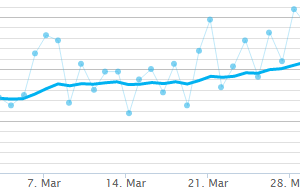
The benefit of CGMs over glucometers is that they’re painless and you don’t need to prick your finger and draw blood, so they’re more convenient. Plus, as the name implies, CGMs detect your glucose level continuously, 24/7, rather than being a one-time measurement. It’s much easier to identify patterns and trends when you can see your glucose level all day and all night, rather than only when you draw a drop of blood.
Because CGMs don’t actually measure blood glucose, CGM and glucometer readings don’t always match up. Readings on a CGM may lag behind a blood measurement by about 5-10 minutes. But even if the exact levels aren’t the same at a given moment, the ballpark level at that time and the general trends – whether glucose is rising or falling – should be similar.
CGM data are typically transmitted to an app on your phone every five minutes, 24 hours a day, and the readings can also be synced with a physician’s office for medical monitoring.
Who should use a CGM? Is it helpful for diabetes?

Anyone interested in optimizing their health can benefit from wearing a CGM. These devices can be a helpful tool to customize your diet because you can clearly see how the foods you choose affect your glucose level. If you follow a keto diet, you might be avoiding foods that would actually work well for you, and on the flipside, you might discover that the “keto bread,” “keto cereal,” “keto granola” and other treats you’ve been enjoying aren’t quite as benign for your blood sugar as they’re marketed to be.
Being able to personalize your diet is a good reason for anyone to wear a CGM, but this can be especially helpful for people with diabetes, particularly if they use insulin. Having a convenient way to check your glucose level makes it easier to adjust insulin doses safely and to see when it may be time to reduce or eliminate other diabetes medications. (Always working with your healthcare provider, of course.)
Benefits of wearing a CGM

CGMs offer several advantages over conventional glucometers. The most obvious is that they’re less time-consuming and tedious, since the sensor is inserted just once and can be worn for a week or two, depending on what device you use. Inserting and wearing the sensor are nearly painless, and there are no additional needles, alcohol swabs, or lancets needed.
CGMs can be helpful for playing detective in cases where someone’s hemoglobin A1c is higher than they would expect based on what they typically eat. As keto and carnivore diets become more popular, more people are reporting this – an A1c level that’s a bit elevated considering their diet contains little to no carbohydrate. Data from a CGM could confirm whether the A1c is truly reflective of the glucose levels, or whether it’s not correlating as well as it’s typically believed to. (The A1c test has some shortcomings that are important to be aware of.)
This can be reassuring if you’re worried that your glucose control isn’t as good as you thought it was, or if your CGM data indicates your glucose is often higher than you expected, then you can use that to fine tune your food choices.
CGMs can help identify patterns

Food isn’t the only thing that affects glucose levels. CGMs can help you see how other factors influence your glucose. For example, stress and poor sleep are both known to result in reduced insulin sensitivity and higher glucose. Seeing those numbers in real time might be the nudge you’ve needed to make lifestyle changes you’ve been resisting.
Fighting off an illness, like an infection or cold, also tends to elevate glucose. Something else that raises glucose in most people is intense exercise. (This isn’t a bad thing, though. When you’re going all-out, your muscles need a bit more glucose to power themselves, so your liver does them the favor of making some.)
On the other hand, low-intensity exercise – like walking – typically lowers blood glucose. This is why it’s recommended that people with diabetes go for a short walk after meals.
Reproductive age women can use CGMs to see how their menstrual cycle affects their glucose levels. Changes in insulin sensitivity and glucose levels throughout the month might help explain food cravings, at least for some women.
Understanding what’s normal in basic human physiology, and learning what’s normal for you, specifically, can ease a lot of worry and clear up confusion when you see glucose levels that seem mysterious.
CGMs can be especially helpful for people living with mental health issues. The near-real-time data can show someone if there’s a connection between their glucose levels and their mood or cognitive function. For example, feelings of anxiety, irritability and panic might not be all “in someone’s head,” but could well be the result of low or rapidly falling glucose.
CGMs also make it easier to see correlations between glucose levels and sugar cravings or dips in energy and focus. Identifying these patterns can help people make food choices that will keep them feeling better not just physically, but also mentally and emotionally. (Read here for more on how keto diets can be beneficial for mental health.)
Drawbacks to wearing a CGM

For most people – especially those with diabetes – the benefits of wearing a CGM far outweigh the drawbacks. But that doesn’t mean there are no negative aspects to CGMs.
If you don’t have a nuanced understanding of normal, healthy blood sugar regulation, then every little rise and fall on a CGM graph can be worry-inducing. You might be alarmed by completely normal fluctuations. If that’s the case, then rather than contributing to better health, a CGM can lead you to increased stress and anxiety.
The same is true for weighing yourself: a scale can provide objective feedback about your body weight that you can use to guide your food choices, or it can wreck you, emotionally, if you use it as the arbiter of your self-worth. A CGM, like a scale, a ketone meter, or any other biosensing device, can be a helpful tool to guide you in making better choices, provided you don’t weaponize it against yourself and hold yourself hostage to every little flicker.
With this in mind, a CGM is a great way to learn about what’s normal. You’ll be able to see for yourself how low- and high- intensity exercise affect your glucose, as well as the impact of stressful situations, poor sleep, and other factors, and of course, your diet. And most CGM apps come with an option for customer support where you can consult with experts to ask questions if there’s something you want to understand better.
Important points to be aware of with a CGM

CGM sensors are most commonly worn on the back of your arm. Placing it there means that you may occasionally roll over it during the night while you sleep.
When this happens, the sensor might not be able to get an accurate reading and it will sound an alarm that your glucose is dangerously low. It’s important to know that this is often a false reading, called a “compression low.” If you feel well, you don’t have diabetes, and you have no symptoms of hypoglycemia, then it’s most likely a compression low and you can disregard it.
But if you have diabetes or you feel unwell, verify the glucose level with a blood measurement using a glucometer. In fact, this instruction is not just for a compression low. Any time you see a reading on your CGM that’s especially high or especially low and you feel unwell, and particularly if you have diabetes and you use insulin, take a blood glucose measurement so you can take corrective action if needed for your safety.
Medical Education
A paper published in 2022 profiled an intriguing project in which medical and dental students from Harvard University wore CGMs for 30 to 40 days. The participants discovered things that led them to alter their own eating habits, and which might have a beneficial influence on how they treat their future patients:
“This experience has definitely changed my eating habits – after seeing how avoiding rice and carbs in general curbed my glucose response, I was more inclined to eat low-carb meals for lunch and dinner… I think my definition of ‘healthy eating’ now includes a sense of foods’ glycemic indices and their associated glucose spikes in a way that it didn’t before.”
“I have also sought to decrease my simple carb intake, as I found that I had dramatic glucose spikes, and subsequent fatigue, when consuming large amounts of simple carbs.”
“I will definitely be thinking about the ways that a CGM could help my patients. Especially those that are struggling with weight or energy throughout the day. [Observing] the graph of what my sugars were doing when I was feeling tired was very informative for what I was consuming and think that it could help my patients too!”
“I definitely think [having worn a glucose monitor] will impact the way I practice medicine. I learned that nutrition is not a cookie cutter science (is any part of medicine, really?) and it needs to be extremely individualized. I would not hesitate to recommend the CGM to my patients so they can learn how their body reacts to different foods.”
How to get a CGM

In the US, some insurance companies cover CGMs for people with diabetes, but some companies may only cover it for people who use insulin. If you don’t have diabetes or don’t use insulin, your doctor can still prescribe a CGM but you’ll need to cover the cost yourself.
The biggest breakthrough with CGMs as of the time of writing is that they’re now available over the counter, so anyone can get one; no prescription is needed.
How Long Should You Use a CGM?

Depending on what model you use, most CGM sensors last 7-14 days. If you’re not using a CGM to inform adjustments to your insulin or other medications, then you don’t need to wear one for months at a time. You can wear one all the time if you want to and you enjoy seeing the data, but wearing one for a few weeks is typically long enough for most people to gather the information they need. (People with diabetes can obviously benefit from wearing one all the time.)
If you like seeing the data now and then but don’t want to use a CGM perpetually, year-round, you can use one a few times a year to check in on yourself and confirm that your diet is still working well for you. And if you want to expand your diet a little and introduce some foods you’ve been avoiding, a CGM can help you experiment to see if those foods would work well for you.
Another good use for a CGM is giving yourself a reality check. If you know you’ve been straying from your low-carb or keto diet, you’ve regained some weight and maybe some health issues have started to reemerge, wearing a CGM for two weeks – just one sensor – can be an effective self-accountability tool to help you get back on track.
Bottom Line

Like most other wearable biotechnology devices, CGMs provide valuable feedback that you can use to inform yourself in making diet and lifestyle changes to support improved health. But it’s important to understand some basics about normal fluctuations in glucose levels so that you can take helpful actions while avoiding unnecessary worry.
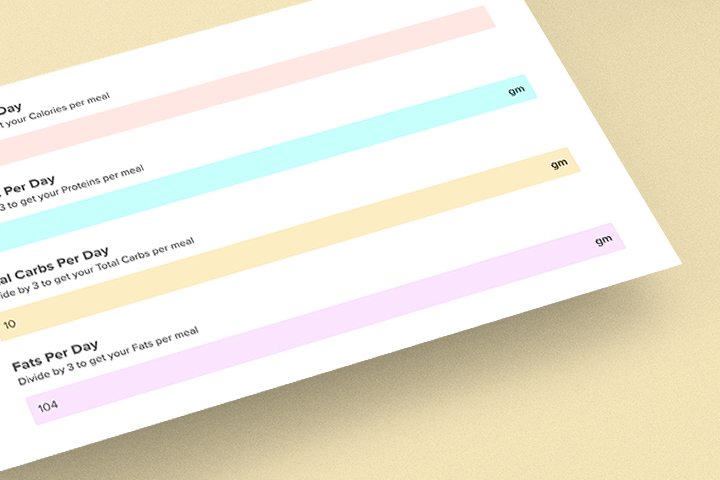
Looking for a low-carb meal?

Then check out Keto Chow! Keto Chow is a meal shake with 1/3 of your daily recommended nutrients; plus, it’s gluten free, keto friendly, and has no added sugar. Choose from over 25 delicious flavors!